Introduction
Fanconi anemia (FA) is an inherited disorder of impaired DNA repair, associated with progressive bone marrow failure (BMF), leukemia, and cancer predisposition. Hematopoietic cell transplantation (HCT) may be curative for FA associated BMF, and changes in HCT practice over the past decades may have impacted outcomes in FA patients.
Methods
We used CIBMTR database to perform a retrospective cohort study of children and adults undergoing first allogeneic HCT for FA BMF (patients with MDS/AML excluded) from 2000-2018. We hypothesized that contemporary HCT approaches, including decreases in radiation and increase in use of serotherapy and ex-vivo graft manipulation, would associate with improved outcomes in FA patients receiving HCT. The primary endpoints were overall survival (OS) and early subsequent malignant neoplasm (SMN; by 5 yr post-HCT). Secondary endpoints included event free survival (EFS; death, SMN or graft failure), treatment related mortality (TRM), graft failure, and acute (grade II-IV) and cGVHD. Univariate and multivariate Cox regression models were created to evaluate the impact of conditioning, donor and graft source, treatment era, and patient characteristics on outcomes, adjusting for other significant covariates. Due to confounding factors, we were not able to create a single multivariate model that included radiation, ex-vivo graft manipulation, and donor and graft source; therefore, we performed subgroup univariate analysis for patients receiving unrelated donor bone marrow (BM) or peripheral blood stem cell (PBSC) HCT.
Results
We analyzed 652 HCTs from 2000-07 (n=353) and 2008-18 (n=293). 223 (35%) patients had a matched related donor (MRD) with any graft type, 244 (38%) had an unrelated donor BM or PBSC grafts, 123 (19%) had an unrelated cord blood graft, and 44 (7%) had a related haploidentical donor with any graft type.
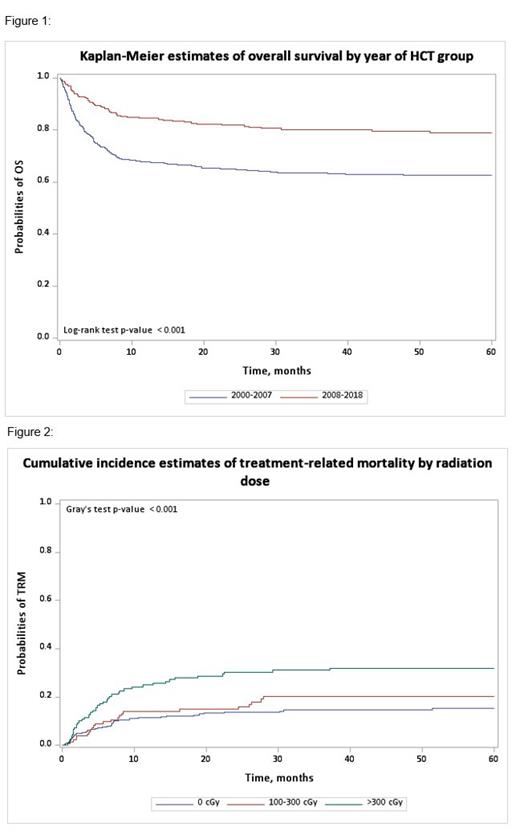
Between the two treatment eras, 5-yr OS has dramatically improved (78.8% 2008-18 v 62.5% 2000-07, p<0.01; figure 1) driven by lower 5-yr TRM (15.2% v 25.5%, p=0.004) and lower rates of primary (7.9% v 12.9% at 42 days, p=0.038) and secondary (4.1% v 8.9% at 1 year, p=0.014) graft failure. No statistically significant change was observed for aGVHD, cGVHD, or early SMN.
Assessing the entire cohort, use of total body irradiation (TBI) >300cGy was associated with lower OS (HR=1.75, 95% CI 1.24-2.47) and increased TRM (HR=3.36, 95% CI 1.54-7.34; figure 2) on multivariable analysis. For patients that received unrelated BM or PBSC HCT, use of TBI was associated with inferior OS survival (HR=1.93, 95% CI 1.18-3.17), EFS (HR=1.78, 95% CI 1.13-2.80), and TRM (HR=2.31, 95% CI 1.20-4.46) on univariate analysis.
Among all patients, CD34 selection or T-cell depletion ( ex vivo depletion) were not associated with better OS (95% HR=1.014, 95% CI 0.84-1.56), EFS (HR=1.163, 95% CI 0.86-1.58), or TRM (HR=0.79, 95% CI 0.52-1.19) but was associated with less aGVHD (HR=0.35 95% CI 0.22-0.57) and lower but not-statistically significant cGVHD (HR=0.54, 95% CI 0.29-1.01) on multivariable analysis. Within the unrelated donor setting, univariate analysis showed reduced aGVHD (HR=0.39 95% CI 0.23-0.68) and cGVHD (HR=0.47 95% CI 0.28-0.79) but did not have a significant effect on OS, EFS, or TRM.
Early SMN occurred in 3.2% of participants by 5-years post-HCT and was associated with cGVHD occurrence (HR=2.14, 95% CI 1.06-4.33) and older age (>18 v <9 years, HR=6.35, 95% CI 2.66-15.14), but not ex-vivo depletion or use of ATG or alemtuzumab. Early SMN risk was not impacted by the use of TBI (HR=1.60, 95% CI 0.77-3.34), but secondary analysis demonstrated a trend towards a relationship with doses >300 cGy (HR=2.24, 95% CI 0.99-5.08).
Conclusions
Outcomes for patients with FA BMF have improved significantly in more recent HCT eras, driven by reductions in TRM and graft failure risk. Although radiation doses >300cGy were associated with greater toxicity, doses of 100-300cGy were not associated with inferior outcomes in our cohort. Use of CD34 selection or T-cell depletion may reduce the risk of GVHD in transplant FA patients, but does not appear to impact 5-yr OS. Risk for early SMN development in FA patients receiving HCT associates with older age and cGVHD.
Disclosures
Rotz:RCI BMT: Other: medical monitor for NMDP. Myers:Incyte: Other: Clinical trial funding; Elixirgen Therapeutics: Other: Industry sponsored clinical trial .

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal